To utilize timestamps to skip to specific sections, click on the video to watch on Youtube’s site.
What is Spondylolysis?
Spondylolysis is similar to a stress fracture, in that it’s a bony defect often as a result of repetitive stress. However, since it doesn’t follow the typical rules for diagnosis and treatment of stress fractures, labeling it as such is contentious.
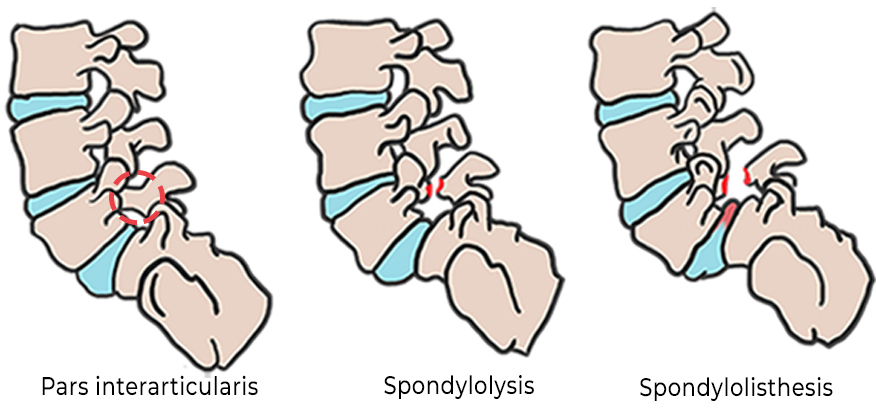
Spondylolysis is located in a specific part of the spine called the “pars interarticularis”, which is why spondylosis often goes by these other names:
- Pars fracture
- Pars stress fracture
- Pars defect
A fracture in this part of the spine significantly increases the risk of spinal instability, with the possibility of progressing into a more serious condition called spondylolisthesis.
Spondylolisthesis is when a vertebral bone slips forward onto the bone directly beneath it, resulting in pain and potential nerve damage.
Although spondylolysis is most commonly found in the lumbar spine (low-back), it can also occur in the cervical and thoracic regions as well (neck and mid-back).
How common is spondylolysis?
Spondylosis has a prevalence of about 3-10% amongst Americans. (1)
The range can be attributed to varying definitions of spondylolysis in the literature.
The literature varies on whether asymptomatic individuals with positive diagnosis on imaging or those with symptoms and negative diagnosis on imaging should be included in the statistics.
Regardless, it is generally agreed upon that It is particularly common in young athletes.
In one study of 532 patients aged 8 or younger who reported general lumbar complaints, 4.7% were diagnosed with spondylolysis.
In a study of 153 patients aged 19 and younger who reported low back pain for 2+ weeks the prevalence increased to 39.7%. (2)
A similar study found the rate as high as 30% among 1025 adolescents who reported low back pain. (3)
All positive diagnoses of spondylolysis in these studies had a history of athletic participation.
Studies have also shown that young athletes with bilateral or chronic pars fractures progress to the more severe condition of spondylolisthesis at a rate as high as 43-74%. (4)

What causes spondylolysis?
Spondylolysis is most commonly a result of repetitive trauma, rather than from a single event.
It is more commonly seen in young athletes who participate in sports which involve frequent lumbar extension (arching your low-back), such as gymnastics or football.
There may also be a genetic component that increases the risk for spondylolysis. It is more commonly found in Caucasians and Inuits.

What are the symptoms of spondylolysis?
Pain and stiffness around the injured vertebral site are common symptom of spondylolysis.
The back pain is most often made worse with bending backwards (lumbar extension).
When should I see a doctor about spondylolysis?
If you are experiencing some of these symptoms, it is recommended that you consult with your physician:
- Back pain associated with major trauma
- Pain that restricts normal movement
- Pain that is associated with numbness, tingling, weakness or neurologic symptoms
- Pain that is present at rest
- Pain at night
- Pain that impacts daily activities
- Pain that does not subside with simple measures like rest, ice, stretching, and ibuprofen
In some cases, there is no history or major trauma; no neurologic findings; no significant impact on physical activity but pain that nonetheless has been present on a regular basis for 2 or more weeks.
This type of back pain should also be evaluated by a physician who is familiar with back pain in young athletes and spondylolysis in particular.
Waiting until the symptoms are more pronounced or disabling is not advised. The earlier a proper diagnosis can be made, the more effective the treatment and the better the outcome.
How is spondylolysis diagnosed?
Typically, first a clinical examination will be conducted to determine the likelihood of a spondylolysis diagnosis. The clinical examination will typically include collecting a patient history to determine risk factors, followed by a physical examination involving palpation and having the patient perform several different movements.
Based on the findings of the clinical examination, the provider may then request additional diagnostic imaging to further inform their diagnosis.
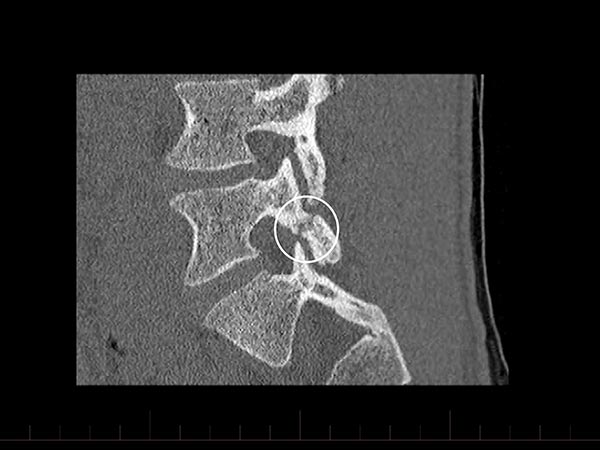
The gold standard used to be a combination of SPECT and computed tomography (CT) scan. However, MRIs are now considered to be the better option as they are faster, cost about the same, require no radiation, and provide more details that may assist in creating a differential diagnosis. (6,7,8)
X-rays are also an option to detect a fractured vertebra.
Below on the left is a CT scan of spondylolysis.
On the right is a MRI scan of spondylolisthesis.

How is spondylolysis treated?
Spondylolysis can often times be treated conservatively.
The primary aims of the treatment are to optimize the body’s ability to heal the fractured bone, improve strength and mobility, and reduce pain.
Common treatments include:
- Physical Therapy
- Reduction or cessation of aggravating activities
- The use of spinal braces to prevent spinal motion and create a more stable environment for the fracture to heal.
- In some rare cases, surgery may be indicated (more info below)
The use of NSAIDs and steroid injections is generally not recommended, due to concerns of bone healing interference.
However, despite the potential impacts to bone healing, some physicians may still prescribe these medications to reduce pain.
How can I reduce my risk for spondylolysis?
It is arguable if spondylolysis risk can truly be reduced. However, it is generally agreed upon that early recognition and treatment can improve outcomes and decrease the risk of long-term complications.
Physical therapy can be helpful through strengthening and mobility exercises, as well as improving rates of recovery. Your therapist should also be able to educate you on proper body mechanics and training intervals to help improve the safety and sustainability of the activity.
Do I need surgery for spondylolysis?
With proper conservative treatment, surgery is rarely indicated for spondylolysis.
The main surgical indication is spondylolisthesis. If there is a bilateral pars defect and if the vertebrae shift forward and are unstable, a surgical fusion may be indicated.
If a spondylolysis fails to heal (non-union, with or without spondylolisthesis), there may be persistent pain and instability which may warrant a surgical consultation.
What happens if I let spondylolysis go untreated?
It is possible that with simply avoiding the aggravating activity and allowing the spine to rest, the fracture will heal and the pain will subside.
However, it is likely that by simply stopping all strenuous activities throughout the recovery, there will be a decrease in strength, endurance, and mobility.
This overall decrease in conditioning can also put an athlete at an increase risk of injury when trying to return to sport.
This is why we recommend working with a physical therapist, who can provide safe exercises to maintain conditioning while also allowing the bone to heal.
If someone were to continue performing the aggravating activity through the injury, it is likely the fracture would continue to worsen, resulting in progressively more intense pain, weakness, and stiffness.
There would also be an increase risk of the spondylolysis developing into a spondylolisthesis and potential nerve injury.
How long does it take to recover from spondylolysis?
Full recovery can take anywhere from a few weeks to a few months, depending on the extent of the injury and different factors of the injured individual themselves.
Although some patients will have pain relief after a few weeks of rest, it typically takes much longer for the spondylolysis to heal and much longer to develop the flexibility, core strength, proper body mechanics, and functional progression for full recovery back to sports training and competition.
A physical therapist will be able to monitor the injury from week to week to optimize the progress. Preferable the therapist will eventually be able to have the patient perform the initial aggravating activity, or an approximation of it, in clinic.
At GO PT, we want to ensure that the patient is able to tolerate the activity in a controlled environment, in order to feel confident that they’ll be able to perform the activity safely and sustainably in the real-world environment.
References:
- T. Lemoine, J. Fournier, T. Odent et al., “The prevalence of lumbar spondylolysis in young children: a retrospective analysis using CT,” European Spine Journal: Official Publication of the European Spine Society, The European Spinal Deformity SocietyEuropean Spine Journal, vol. 27, no. 5, pp. 1067–1072, 2018.
- A. Nitta, T. Sakai, Y. Goda et al., “Prevalence of symptomatic lumbar spondylolysis in pediatric patients,” Orthopedics, vol. 39, no. 3, pp. e434–e437, 2016.
- M. Selhorst, A. Fischer, and J. MacDonald, “Prevalence of spondylolysis in symptomatic adolescent athletes: an assessment of sport risk in nonelite athletes,” Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine, 2017.
- C. H. Crawford, C. G. T. Ledonio, R. S. Bess et al., “Current evidence regarding the etiology, prevalence, natural history, and prognosis of pediatric lumbar spondylolysis: a report from the Scoliosis Research society evidence-based medicine committee,” Spine Deformity, vol. 3, no. 1, pp. 12–29, 2015.
- Sara Goetzinger, Selen Courtney, Kathy Yee, Matthew Welz, Maziyar Kalani, Matthew Neal, “Spondylolysis in Young Athletes: An Overview Emphasizing Nonoperative Management”, Journal of Sports Medicine, vol. 2020, Article ID 9235958, 15 pages, 2020. https://doi.org/10.1155/2020/9235958
- Gunzburg R., Szpalski M., Spondylolysis, Spondylolisthesis and Degenerative Spondylolisthesis, Lippincott Williams and Wilkins, 2006, p. 21.
- Depalma M.J., iSpine: Evidence-based interventional spine care, Demos Medical Publishing, 2011, p. 156-157.
- Hyde TE. Spine-health. Profile and Diagnosis of Spondylolysis. http://www.spine-health.com/conditions/spondylolisthesis/profile-and-diagnosis-spondylolysis